There’s much debate about what recovery looks like.
In fact, in some fun videos on Instagram (https://www.instagram.com/mikeandguida/) and Facebook (https://www.facebook.com/MikeAndGuida) that I do with my friend, the renowned trainer Mike McGowan, we recently talked about “California Sober,” and sheesh, did we get pushback!
For the unfamiliar, “California Sober,” according to one source, means “when a person gives up on alcohol and hard drugs but continues to consume marijuana. Some individuals also permit the use of psychedelic drugs, such as ayahuasca, LSD or magic mushrooms. This approach has gained popularity in recent years, becoming somewhat of a buzzword in recovery circles” (Castle).
The argument is that, since cannabis (and most hallucinogens) are not fatal from the perspective of overdose, they save lives compared to opioids. But cannabis and hallucinogens are not prescribed by a reputable doctor to treat substance use disorders (SUDs) because there’s no evidence that they work to do so (NCBI). Further, recovery is a continuum, not an end goal. It takes daily work; social support, often in the form of 12-step meetings or talk therapy; and physical effort.
There are drugs — mood-altering, prescribed drugs — used to treat SUDs: methadone and buprenorphine treat opioid use disorder; benzodiazepines treat alcohol withdrawal; gabapentin treats alcohol use disorder, but mostly it treats alcohol withdrawal (JAMA). And that’s where the conflict enters. The 12-step movement has a long-standing bias against medication for addiction treatment (MAT). I’m not here to criticize it, but I admit that I don’t understand it. From Tradition Three of Alcoholics Anonymous, “The only requirement for A.A. membership is a desire to stop drinking” (AA). Narcotics Anonymous says basically the same thing: “There is only one requirement for membership, the desire to stop using” (Wisconsin). So if I can join by virtue of wanting to stop drinking or using, how does my medication, taken as prescribed and not making me high, make me less deserving of recovery?
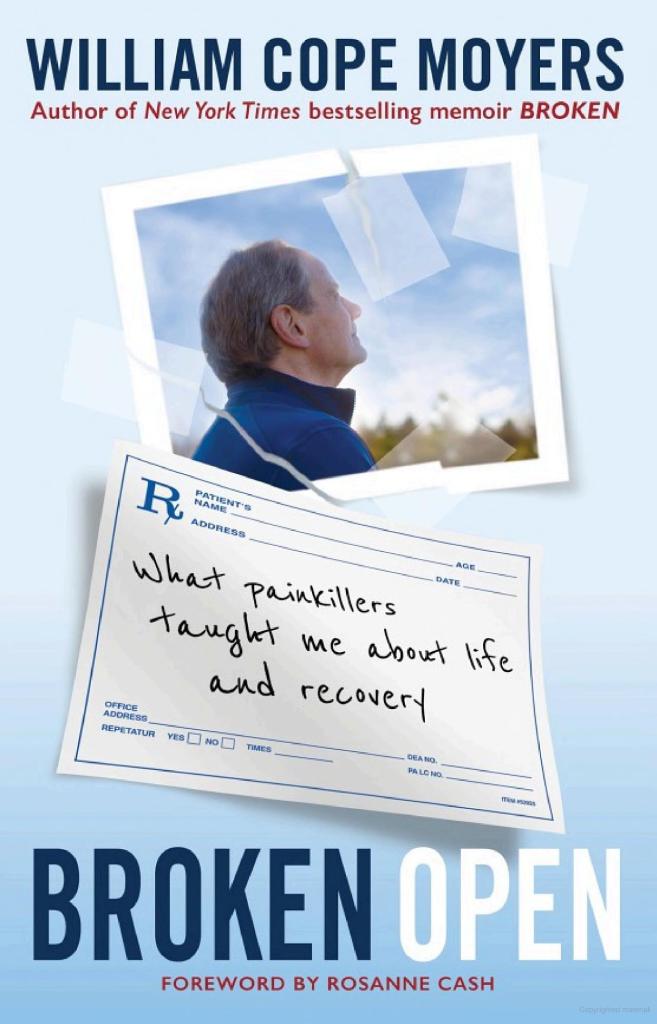
I contend it doesn’t. Bestselling author William Moyers writes in his memoir, Broken Open, about “the triad of abstinence, sobriety, and recovery,” and how “urgently I needed to figure out how my new experience of recovery [after being prescribed Suboxone] aligned with those practical principles” (Hazelden). He figured it out, and his book is a great explanation of addiction, opioids, and recovery. He likens addiction to breast cancer, and quotes Dr. Frenz, “Breast cancers can have mutations that make them resistant to some medications. Treating cancer requires a very specific and individualized approach. We tend to lump substance use together, but they are different because the drugs are different” (Hazelden).
While Moyers writes, and I agree, “Purity isn’t the point — this is about staying alive” (Hazelden), “California Sober” is different, at least in my mind. Aside from being insulted and sworn at by strangers who disagree with us, the arguments for “California Sober” were essentially that cannabis is harm reduction, which saves lives, and therefore cannabis is fine to use in all its forms. Oh, and there were lots of “one time at band camp” stories about how cannabis use is helping a specific individual overcome addiction.
And I’m sure those individuals are telling the truth. But the points remain the same: harm reduction is still harm; addiction can’t be siloed to specific drugs; “California Sober” isn’t using a drug as prescribed to treat a substance use disorder; it’s getting high more safely than with opioids.
In 2007, recovery was defined as “a voluntarily maintained lifestyle composed (sic) characterized by sobriety, personal health, and citizenship” (NAADAC).
More recently, in 2024, SAMHSA described The Four Major Dimensions of Recovery: “Health – Overcoming or managing one’s disease(s) or symptoms — for example, abstaining from use of alcohol, illicit drugs, and non-prescribed medication if one has an addiction problem — and for everyone in recovery making informed, healthy choices that support physical and emotional well-being; Home – Having a stable and safe place to live; Purpose – Conducting meaningful daily activities, such as a job, school volunteerism, family caretaking, or creative endeavors, and the independence, income, and resources to participate in society; and Community – Having relationships and social networks that provide support, friendship, love, and hope” (SAMHSA). The emphasis is mine, because we don’t argue definitions.
Cannabis isn’t medicine except in the following limited situations, and even then, I implore someone to tell me when it is smoked that it goes from therapeutic to high-making. (Spoiler: You can’t. There are far too many factors to consider, making the task impossible except on a VERY personalized basis.):
“There is conclusive or substantial evidence that cannabis or cannabinoids are effective:
- For the treatment of chronic pain in adults (cannabis)
- As antiemetics in the treatment of chemotherapy-induced nausea and vomiting (oral cannabinoids)
- For improving patient-reported multiple sclerosis spasticity symptoms (oral cannabinoids)
“There is moderate evidence that cannabis or cannabinoids are effective for:
- Improving short-term sleep outcomes in individuals with sleep disturbance associated with obstructive sleep apnea syndrome, fibromyalgia, chronic pain, and multiple sclerosis (cannabinoids, primarily nabiximols)
“There is limited evidence that cannabis or cannabinoids are effective for:
- Increasing appetite and decreasing weight loss associated with HIV/AIDS (cannabis and oral cannabinoids)
- Improving clinician-measured multiple sclerosis spasticity symptoms (oral cannabinoids)
- Improving symptoms of Tourette syndrome (THC capsules)
- Improving anxiety symptoms, as assessed by a public speaking test, in individuals with social anxiety disorders (cannabidiol)
- Improving symptoms of posttraumatic stress disorder (nabilone; a single, small fair-quality trial)
“There is limited evidence of a statistical association between cannabinoids and:
- Better outcomes (i.e., mortality, disability) after a traumatic brain injury or intracranial hemorrhage” (NCBI).
And if you find a Dr. FeelGood to prescribe cannabis to overcome addiction, know that “There is no evidence to support or refute the conclusion that cannabinoids are an effective treatment for achieving abstinence in the use of addictive substances” (NCBI). That is, you can’t use a non-prescribed medication under the pretense that you’re overcoming your addiction, then say you’re sober or in recovery. Well, you can, but you’re only lying to yourself.
References
https://www.hazelden.org/store/item/560325?Broken-Open
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2762700
Leave a comment